London Food Allergy & Intolerance Testing
Identify Your Food Triggers with Confidence
Find out what may be causing your child’s symptoms with our reliable testing. Our service helps you learn more about the body’s reactions to certain foods to make informed decisions about your diet and lifestyle.
★★★★★
“Dr du Toit is a fantastic specialist, my son and I both very much respect and value his expertise. We have seen many doctors over the years and Dr du Toit is one of those special doctors that can really make a difference in a person’s life.”
Understanding Food Allergies and Intolerances
While the terms "food allergy" and "food intolerance" are often used interchangeably, they are distinct conditions with different underlying mechanisms:
➙ Food Allergy: A food allergy is an adverse immune response to a specific protein, usually mediated by Immunoglobulin E (IgE). When someone with a food allergy consumes a trigger food, their body releases histamine and other chemicals, leading to a range of symptoms that range from mild to life-threatening. Common food allergens include peanuts, tree nuts, sesame, milk, eggs, soy, wheat, fish, and shellfish.
➙ Food Intolerance: A food intolerance involves the digestive system and does not involve IgE. It occurs when the body has difficulty digesting a particular food (usually a carbohydrate) due to enzyme deficiencies or sensitivities to certain food additives, e.g. sulphites. Symptoms of food intolerance are troubling but typically less severe than those of a food allergy and may include bloating, gas, diarrhoea, growth failure and abdominal pain.
Why Get Tested?
Identifying triggers that are relevant to you or your child - through food allergy and intolerance testing - is essential for several reasons:
➙ Accurate Diagnosis: Pinpointing the specific foods causing your symptoms allows for targeted dietary elimination, safe dietary expansion and appropriate management strategies which may include Oral Immunotherapy.
➙ Improved Health: By avoiding trigger foods, you can reduce or eliminate allergy symptoms, improve overall health and growth in children, and enhance quality of life.
➙ Peace of Mind: Knowing of relevant triggers empowers you to make informed food choices and confidently navigate situations involving food, e.g. travel, school catering, sleepovers, university, and eating out socially
➙ Prevent Severe Reactions: In the case of food allergies, early diagnosis and management are crucial to prevent life-threatening allergic reactions (anaphylaxis).
Why Choose London Allergy Consultants?
London Allergy Consultants stands out as a leading provider of food allergy and intolerance testing in London. Here's why you should choose us:
-

Comprehensive Testing
We offer a wide range of tests, including skin prick testing, specific IgE blood testing, and component-resolved diagnostics.
-

Expert Consultants
Our team of experienced allergists is dedicated to providing personalised care and support.
-

Patient-Focused Approach
We prioritise your comfort and well-being, creating a welcoming and supportive environment.
-

Advanced Technology
We utilise the latest technology and techniques to ensure accurate and reliable results.
-

Convenient Location
Our clinic is conveniently located in London, with easy access to public transportation.
Common Conditions Related to Food Allergies
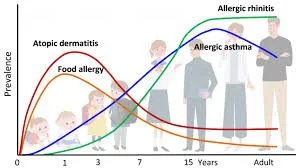
Food allergies can often be associated with other allergic conditions; these may develop in a sequence known as the allergic march, typically commencing with infant eczema, followed by food allergies, asthma, and hay fever. Other conditions include:
➙ Allergy Rhinitis: Also known as hay fever, this condition involves inflammation of the nasal passages due to allergens like pollen, pet dander and house dust mites. HDM gives rise to perennial symptoms like eczema flares (especially of exposed skin areas), early morning sneezing and nasal blockage, allergic coughing, and itchy eyes.
➙ Allergic Asthma: This chronic respiratory condition can be triggered by aeroallergens. Most children with persistent asthma will be allergic to one or more aeroallergens. Patients with active asthma are at greater risk of severe food-induced allergic reactions.
➙ Primary and Secondary Food Allergies: Primary, e.g. cashew nut allergy typically develops early in life and is associated with more severe reactions. Secondary food allergies develop in children who become allergic to pollen. This is also known as oral allergy syndrome or pollen food syndrome, which arises as certain pollens and certain foods share these proteins. These reactions are typically milder and do not occur if the food is heated or cooked.
Types of Food Allergy and Intolerance Tests
-

Skin Prick Testing
This common test involves placing a small amount of the suspected allergen on the skin and pricking the area. A positive reaction, indicated by a raised wheal and redness, suggests an allergy.
-

Specific IgE Blood Testing
This blood test measures the levels of antibodies (IgE) to specific foods in your blood. Elevated IgE levels indicate an allergic sensitisation.
-

Food Intolerance Testing
Used to identify non-allergic food reactions that may cause digestive or skin symptoms. Often guided by elimination diets or targeted testing based on your symptoms.
Our Testing Process
1. Initial Consultation
During your first visit, we discuss your child's symptoms and medical history to determine the right test for you. This is usually followed by a clinical examination looking for eczema, hayfever and asthma features. Growth is measured.
2. The Test
You will be given a clear explanation of any testing to be undertaken. Our tests are carried out in a safe, comfortable, and child-friendly environment. A numbing cream will be offered before blood testing.
3. Review of Results
Once your results are ready, a team member will explain them. Skin test results are available in 15 minutes, and blood allergy tests will take a few days to return. We will then discuss options available to you regarding the allergies suggested by the testing.
4. Follow-Up Support
A follow-up appointment is standard to answer any questions after you receive your results. This will usually be done remotely, but you can attend a face-to-face follow-up.
Treatment Options
The default treatment for food allergies and intolerances has traditionally been avoiding trigger foods and carriage of a bespoke emergency plan and medications. Other management strategies are increasingly available, and we offer:
➙ Allergy Emergency Medications: Antihistamines can help relieve mild allergic symptoms like itching and hives. Epinephrine auto-injectors (such as EpiPen) are essential for treating anaphylaxis, a life-threatening allergic reaction. Newer devices such as Neffy (EurNeffy) will be available in the UK in 2025, and this device will administer adrenaline as an intranasal spray.
➙ Dietary Modifications: Working with a registered dietitian to develop a balanced and nutritious diet that avoids trigger foods is crucial for managing food allergies and intolerances. A dietitian can help you identify suitable alternatives and ensure you're meeting your nutritional needs. This intervention is especially important for allergic children.
➙ Oral Immunotherapy (OIT): This treatment involves gradually increasing exposure to the food allergen under medical supervision to desensitise the immune system. OIT can effectively reduce the likelihood and severity of allergic reactions over time.
➙ Sublingual Immunotherapy (SLIT): Similar to OIT, the allergen is administered under the tongue. SLIT is another option for desensitising the immune system to food allergens.
➙ Biologic therapies such as Omalizumab (Xoliar): This injectable medication has long been used for asthma but is now repurposed to moderate food allergies. It can be taken continuously to reduce the chance of allergic reactions or as cover whilst multi-food OIT is undertaken.
London Allergy Consultants: Your Partner in Allergy Care
At London Allergy Consultants, we provide comprehensive allergy and intolerance testing services in a comfortable, supportive and child-friendly environment. Our experienced consultants will work with you to:
➙ Identify your food and aero-allergy triggers: We offer a range of contemporary evidence-based tests to accurately diagnose food allergies and intolerances.
➙ Develop a personalised management plan: We will help you create a dietary and emergency plan to avoid triggers and manage your symptoms effectively.
➙ Provide ongoing support: We offer education, Dietetic and Psychology resources, and follow-up care to help you live a full and healthy life.
Allergy Blog – Latest Insights & Advice
Stay Informed on Allergy Research & Treatments
Our blog provides expert advice, the latest research, and practical tips on managing allergies effectively.
Our Locations – Accessible Clinics Across London & Surrey
We provide expert allergy care at multiple locations, ensuring convenient access to specialized treatment for food and airborne allergies.
The Portland Hospital – Marylebone
📍 Address: 205-209 Great Portland Street, London, W1W 5AH
ENT4Kids – Wimpole Street, London
📍 Address: 61 Wimpole Street, London,
W1G 8AH
The Allergy Centre Of
Excellence
📍 Address: 10 Duchess Str, Marylebone,
W1B 9AB
Surrey – New Malden Diagnostic Centre
📍 Address: 171 Clarence Avenue, New Malden, KT3 3TX
Frequently Asked Questions
-
Only two validated tests reliably diagnose immediate-onset food allergies: the Skin Prick Test and Specific IgE blood testing. At London Allergy Consultants, we use the Phadia Standardised IgE System for accuracy. Other tests available outside research settings lack predictive value and aren't recommended in ethical clinical care.
-
Specific IgE antibodies are produced in the bone marrow, circulate in small amounts in the blood, and are concentrated in tissues—making skin tests especially useful. However, both methods provide unique insights. For example, high total IgE (common in children with eczema or of African or Asian descent) can complicate blood test interpretations, making skin tests more reliable in many cases.
-
No. Skin prick test results are measured in millimetres (mm), while IgE tests are measured in kU/L. A 5mm result for egg is not directly comparable to 5mm for peanut. Likewise, IgE values differ in significance depending on the allergen.
-
Not necessarily. Test size predicts the likelihood of a reaction—not its severity. However, component testing using advanced allergen technology can provide deeper insight into risk, cross-reactivity, and the likelihood of outgrowing an allergy.
-
Yes. A decrease in test size over time often suggests the allergy is resolving. Low values at initial diagnosis also suggest a higher chance of outgrowing the allergy.
-
Immunotherapy (e.g., sublingual immunotherapy) gradually desensitises the body to allergens. More about SLIT can be found here.
-
Yes. Stop antihistamines at least 3 days prior to testing, as they affect Skin Prick Test accuracy. However, asthma medications and corticosteroids can be continued. Many paediatric cough or sleep medicines also contain antihistamines, so check labels carefully.
-
Absolutely. Even infants can undergo skin or blood tests. Positive results indicate existing allergies and help prevent reactions. Negative results offer peace of mind and help expand the diet safely.
-
Yes. Familiar faces, distractions (e.g., toys, iPads), and referring to Dr Du Toit as “Dr George” can help children feel more at ease. Reward systems (like stickers) also reduce anxiety—useful for both kids and adults!
-
Skin tests are typically itchy but not painful. Blood tests involve a small prick, and we use numbing cream when needed. Both methods are very safe, with rare side effects like local swelling or faintness.
-
Dr Du Toit will create a personalised emergency plan based on the allergy diagnosis. This includes guidance on medications like antihistamines or adrenaline auto-injectors and travel advice. You'll also receive BSACI-approved documentation for schools, carers, and airlines.
-
Yes. The Anaphylaxis Campaign UK provides detailed resources on managing allergies in school settings. View their guidelines here.
-
A healthy maternal diet, early but appropriate food introduction, and breastfeeding can all help reduce allergy risks. Dr Du Toit can advise on tailored prevention strategies during your consultation.
Book Your Appointment Today
If you or your child is experiencing food allergy symptoms or intolerance, don't hesitate to contact London Allergy Consultants. Our team is dedicated to helping you achieve optimal health and well-being.